 Keratoconus
Keratoconus
Eye allergies are overreactions of the body’s immune system when certain substances come in contact with the eyes of sensitive individuals.
These allergy-causing substances (called allergens) can include dust, pollen, mold and
animal dander. Certain ingredients in cosmetics and eye drops also can cause eye allergies in some individuals.
Eye allergy signs and symptoms
The most common signs and symptoms of eye allergies include red eyes, swollen eyelids,
itchy eyes and excessive tearing.
Eye allergy treatment
Avoidance.The best way to handle eye allergies is to
avoid exposure to known allergens that are causing your problems. For example, if animal dander appears to be the
problem, don’t allow your pet in your bedroom and avoid touching your eyes after handling your pet. Also, purchase a
high-quality furnace filter that traps airborne pet dander.
Medications.If you’re not sure what’s causing your
eye allergies, or you’re not having any luck avoiding known allergens that are causing problems, use
doctor-recommended medication to alleviate your eye allergy symptoms.
Over-the-counter and prescription medications each have their advantages; for example,
over-the-counter products often are less expensive, while prescription ones usually are stronger and might be more
effective.
Eye drops are available as simple eye washes, or they may have one or more active
ingredients such as antihistamines, decongestants or mast cell stabilizers to relieve allergy symptoms or reduce the
severity of allergic reactions. Antihistamines relieve many symptoms caused
by airborne allergens, such as itchy, watery eyes, runny nose and sneezing.
Decongestantsclear up redness. They contain
vasoconstrictors, which make the blood vessels in your eyes smaller, lessening the apparent redness. They treat the
symptom, not the cause.
In fact, with extended use, the blood vessels can become dependent on the vasoconstrictor
to stay small. When you discontinue the eye drops, the vessels might actually get bigger than they were in the first
place. This process is called rebound hyperemia, and the result is that your red eyes worsen over time.
Some products have ingredients called mast cell stabilizers,
which alleviate redness and swelling. Mast cell stabilizers are best taken prior to allergy symptoms to reduce your
sensitivity to problematic allergens and can provide long-lasting relief.
Other medications used for eye allergies include non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids.,
In some cases, combinations of medications may be used.
Immunotherapy.You also might benefit from
immunotherapy, in which an allergy specialist injects you with small amounts of allergens to help your body
gradually build up immunity to them.
Eye allergies and contact lenses
Even if you are a successful contact lens wearer, allergy season can make your contacts
uncomfortable. Airborne allergens can get on your lenses, causing discomfort.
Allergens also can stimulate the excessive production of natural substances in your tears
that bind to your contacts, adding to your discomfort and allergy symptoms.
Ask your eye doctor about eye drops that can help relieve your symptoms and keep your
contact lenses clean. Certain drops can discolor or damage contact lenses, so ask your doctor first before trying
out a new brand.
Another alternative is daily disposable contact lenses, which are designed to be worn once,
and then discarded at the end of the day. Because you replace them daily, these lenses are unlikely to develop
irritating deposits that can build up over time and cause or heighten allergy-related discomfort.
Article ©2011 Access Media Group LLC. All rights reserved. Reproduction other than for one-time personal use
is strictly prohibited.
 1802 Paper Mill Road, Wyomissing, PA 19610
1802 Paper Mill Road, Wyomissing, PA 19610


 Keratoconus
Keratoconus Keratoconus
Keratoconus



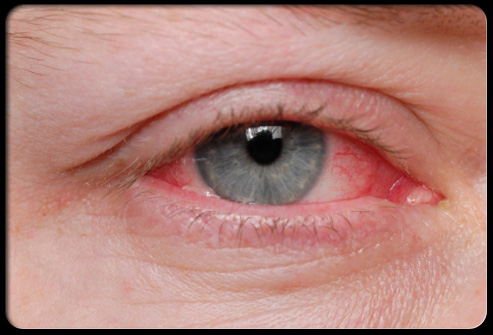
 “Pink eye”, or conjunctivitis, is condition that has likely impacted us all at one point or another but still holds a level of mystery for many. What are its causes and treatments? First, let’s understand what is meant by the words “pink eye”. In case you haven’t yet experienced it, when you have pink eye, your eye becomes pink or red because it’s irritated or inflamed. We all have a thin membrane that covers the inside of our eyelids and the whites of our eyes – it’s called the conjunctiva. When it becomes inflamed or irritated, we have a case of conjunctivitis.
“Pink eye”, or conjunctivitis, is condition that has likely impacted us all at one point or another but still holds a level of mystery for many. What are its causes and treatments? First, let’s understand what is meant by the words “pink eye”. In case you haven’t yet experienced it, when you have pink eye, your eye becomes pink or red because it’s irritated or inflamed. We all have a thin membrane that covers the inside of our eyelids and the whites of our eyes – it’s called the conjunctiva. When it becomes inflamed or irritated, we have a case of conjunctivitis.