Celebrate Summer with a Fresh new look by visiting Berks Eye Physicians and Surgeons for a new pair of prescription sunglasses! Stop in between now and Labor Day and Save 20% off prescription sunglasses! Call us at 610.372.0712 or request an appointment online. See you soon!
Blog
Fossil Eyewear For Men, Now At Berks Eye!
Berks Eye Physicians and Surgeons are proud to announce the addition of Fossil Eyewear for men to our optical boutique. At Fossil, they love all things vintage. It’s true. But it’s not just the look, it’s the feeling you get when something is so uniquely designed that it becomes timeless. And when that feeling or memory resonates with you personally, it’s golden. So it’s no wonder that’s exactly what Fossil was going for with their men’s eyeglass frames! They’re simply the most iconic frame shapes in men’s fashion eyewear.

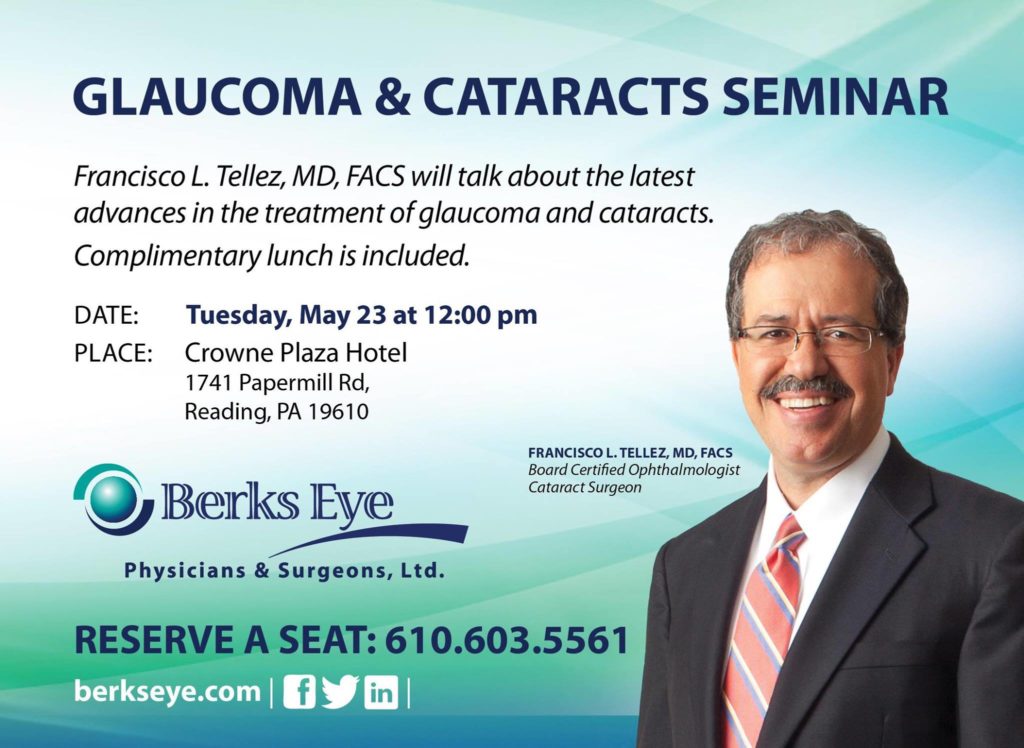
Glaucoma And Cataracts Seminar Hosted By Dr. Francisco Tellez
Dr. Domenic Izzo Wins People’s Choice 8th Year In A Row!

Berks Eye Begins Implanting Micro-stent For Patients With Cataracts And Glaucoma

FOR IMMEDIATE RELEASE
Press Contact: Kathy Bell
610-603-5559
BERKS EYE PHYSICIANS AND SURGEONS BEGINS IMPLANTING LATEST MICRO-STENT DEVICE FOR PATIENTS WITH CATARACTS AND GLAUCOMA
[Wyomissing, PA] – April 24, 2017 –Berks Eye Physicians & Surgeons Ltd. announced that they are now implanting the new Alcon CyPass® Micro-Stent, a micro invasive glaucoma surgical device. It is used to treat patients with mild to moderate primary open-angle glaucoma in conjunction with cataract surgery. Studies have shown the new FDA approved device provides a statistically significant decrease in post-surgical intraocular pressure.
Dr. Peter D. Calder, who was the first board-certified ophthalmologist in the area to implant the device, has seen a reduction in eye pressure after surgery for these patients. Berks Eye Physicians and Surgeons’ other cataract surgeons, Dr. Domenic C. Izzo, Jr. and Dr. Francisco L. Tellez, who is also a fellowship-trained glaucoma specialist, expect to be doing CyPass® Micro-Stent implants in the next several weeks.
Dr. Calder said, “With implantation of CyPass®, many patients will need less medicine to control their eye pressure and some may not need prescription eye drops at all.” The CyPass® Micro-Stent is implanted during cataract surgery, just below the surface of the eye, and is designed to lower eye pressure by enhancing aqueous outflow through one of the eye’s natural drainage pathways. Lowering the pressure inside of the eye is important to protect the optic nerve and to preserve vision in patients with glaucoma.
Dr. Calder’s Active Aging Seminar

Dr. Calder’s Feedback Radio On Weeu.
Glaucoma And Cataracts Seminar With Dr. Tellez
Dr. Peter Calder Speaks About Cataracts, Glaucoma And Chronic Dry Eye
Dr. Peter Calder delivered a powerful and informative seminar over the weekend at the Crowne Plaza Hotel in Reading, PA. Cataracts, Glaucoma, and Chronic Dry Eye were the main focus of Dr. Calder’s educational lecture. A few of the seminar’s highlights we digitally captured and are displayed in the images below. We hope to see you all at our next educational seminar.




Berks Eye Low Vision Open House
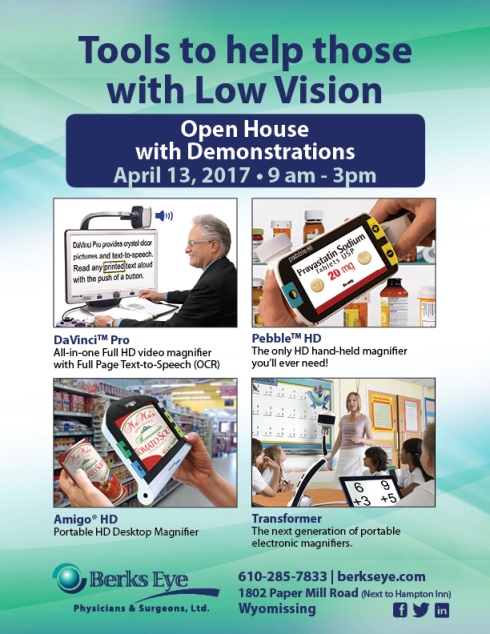
 1802 Paper Mill Road, Wyomissing, PA 19610
1802 Paper Mill Road, Wyomissing, PA 19610